Pediatric dentists are the obvious ones to help children breathe, sleep, and prosper!
Dr. William M. Hang shows how airway health can affect children throughout their life.
Dr. William M. Hang explains why pediatric dentists should be leaders in airway health
Did you know that very young children with reduced oxygen saturation during sleep can suffer from brain damage that can be irreversible?1 You might also be surprised to learn that these same children are more likely to have high blood pressure as adults.1
Breathing problems have been correlated with effects on overall health for more than 100 years.2 Journals from the late 1800s and early 1900s show that our profession realized that altered rest oral posture (which includes mouth breathing) caused changes to facial development and had an adverse effect on overall health. Very early treatment in the primary dentition was encouraged. Articles in respected journals discussed why and how to treat these problems orthodontically.3 Unfortunately, early voices advocating for the benefits of early treatment to establish nasal breathing were drowned out by a chorus of influencers who believed that dentists and orthodontists should focus exclusively on straightening teeth in adolescence. This is pretty much the current paradigm with a few exceptions.
Current status of airway in dentistry
The October 2017 ADA position statement4 recommending that dentists screen for airway issues brought sleep and breathing issues to our attention again. The White Paper from the AAO meeting on Airway and Orthodontics in January 2019, however, minimized the connection between orthodontics and airway. The late Dr. Christian Guilleminault had over 400 articles in the refereed literature and was arguably the most well-known name in the medical sleep arena until his death. He spoke at that AAO meeting but was not one of the authors of the White Paper the AAO published. He cited important medical reasons to recognize and treat airway problems as soon as they are recognized. He particularly cited the high incidence of breathing/sleep problems with premature babies and how waiting to treat them means accepting permanent damage to their health. The most recent AAO annual meeting in Orlando, Florida, featured 237 lectures with only five mentioning the word “airway” in the title. None of those specifically mentioned treatment of children in the primary dentition when many of the children Guilleminault referenced are first diagnosed with problems. If orthodontists are not recognizing and treating these problems in the primary dentition who is going to assume this responsibility?
Pediatric dentists are the obvious group to assume leadership in airway health
Orthodontists get little to no training in working with very young children and are not behaviorally the best trained professionals to deal with children in the primary dentition. Pediatric dentists are trained specifically to work with very young children and are the obvious group to assume a pivotal role in treating the airway pandemic which Guilleminault and others have described. Most pediatric dentists have well established referral patterns with pediatricians and are used to collaborating with that critical group in the medical profession. Clearly there is a gap between medicine and dentistry that should be bridged by the pediatric dentists. If they don’t act, who is left to help these very young children?

Airway health and young children – one case
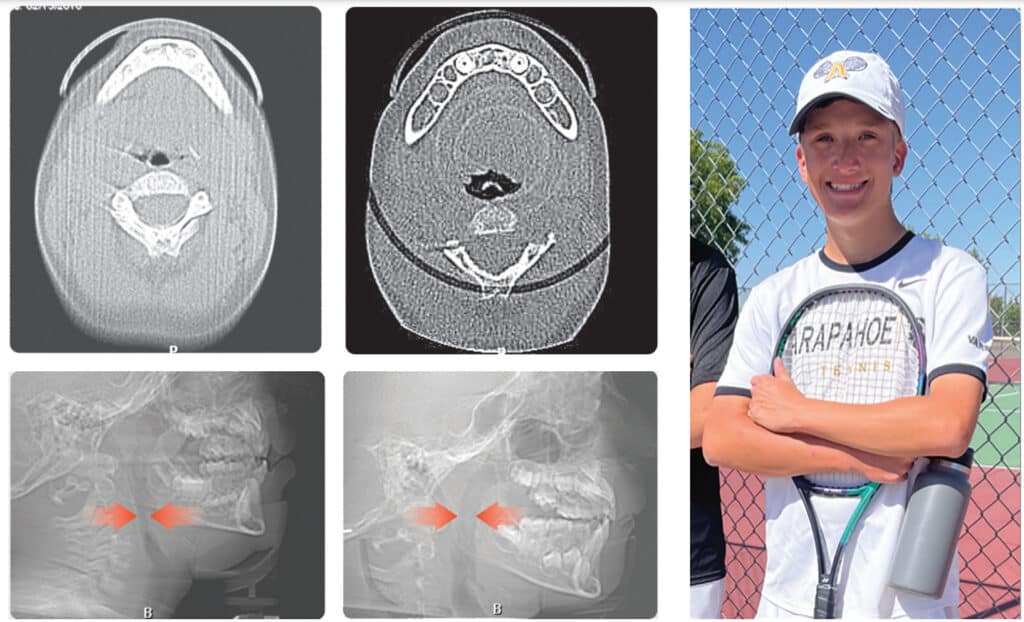
Over 10 years ago, we began Orthotropic® treatment for a 5 year, 3-month-old boy with a diagnosis of Pierre-Robin Sequence, Obstructive Sleep Apnea (OSA), and Failure to Thrive (Figure 1). With lack of forward development of the face commonly seen in Pierre-Robin patients, his airway was compromised, resulting in OSA. The Failure to Thrive diagnosis likely resulted from insufficient growth hormone being released during the deeper stages of sleep. This treatment began before any permanent teeth erupted. Our goal was to eliminate OSA.
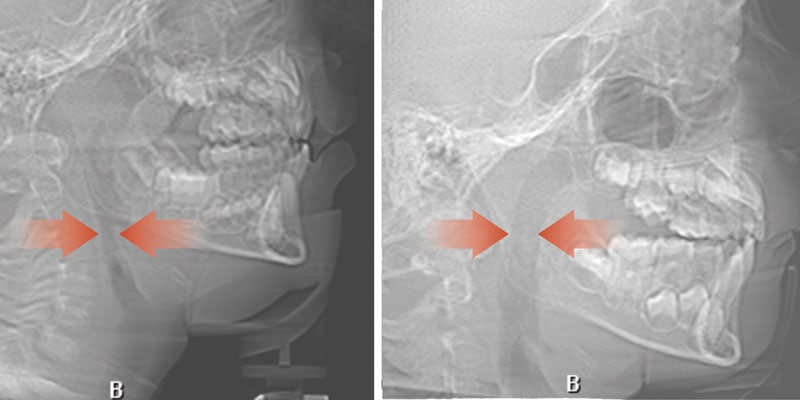
Orthotropics® uses removable appliances to laterally expand the upper arch while simultaneously advancing the upper anterior teeth to their proper place in the face. Then the mandible is developed forward. Orthotropics® is my preferred treatment in cases like this because it negates the head gear-effect producing better facial balance5 and also can result in substantial airway improvements (Figure 2).6
This young boy had great parental support and was very compliant during the treatment. A posttreatment sleep test showed no signs of sleep apnea.7 Failure to Thrive was also overcome. Now at 17 years old, this patient is 5 ft. 7in. tall and is still growing. I believe that improved breathing and sleep has resulted in an increase in HGH production which allowed him to resume normal growth. He’s an aggressive tennis player with a big smile and no return of his OSA (Figure 3). Thankfully, he’s an excellent student with no evidence of brain damage from his early OSA diagnosis.
How hard is it to recognize airway issues?
I’ve had some orthodontists lament that they can’t get really young children to open their mouths for an
examination. The ironic thing is that airway problems can be recognized without the patient even opening the mouth! Lip-apart posture, an accentuated cupid’s bow appearance of the upper lip, a flaccid rolled-out lower lip, crusty lips, mentalis muscle strain to close the lips, flat cheeks, narrow nostrils, forward head posture, or a tilted back forehead are common physical signs of an airway issue and all are obvious without having a child open the mouth. In reality, a properly taken medical history for children this age frequently raises suspicion about sleep/breathing problems and doesn’t require having a child open the mouth. Pediatric dentists are the masters at getting kids to open their mouths and may be able to get an even more complete picture of a child’s dentofacial development as it relates to sleep/breathing than other groups in the dental profession.
Dr. Stephen Sheldon, former director of the Sleep Medicine Center at Lurie Children’s Hospital in Chicago, says, “The identification of disordered sleep really rests on asking the right questions and being able to interpret the answers, and that really begins with all child healthcare professionals.”8 Pediatric dentists are in a perfect position to learn to recognize the signs and symptoms of these problems which can easily be incorporated into every pediatric dentist’s initial examination. If a patient like the one I’ve referenced in this article can be successfully treated, what about other children who may have other symptoms which indicate that they may not be sleeping and breathing well? They exist in virtually every dental practice that treats children.
Brain damage isn’t the only thing that may be prevented by treating the airway. Bedwetting often resolves after sleep and breathing issues are alleviated. Parents also report that there are fewer colds and ear infections, as well as calmer children who are better able to focus on tasks. According to a national 2016 survey, 6.1 million children are diagnosed with ADHD.9 Dr Sheldon says he doesn’t believe there is such a thing as ADHD. He believes it is always a sleep and breathing issue.10 If there are ways to treat this problem, does it make sense that we continue to have a growing percentage of our young children placed on Ritalin and other drugs for ADHD? Normalizing growth and eliminating possible negative effects of untreated sleep apnea should be at the top of the list of must-haves for our growing number of patients who present very early with symptoms of possible sleep and breathing problems. Waiting for permanent teeth to erupt to treat a health problem makes no more sense than waiting for growth to be complete before getting eyeglasses for a child with impaired vision.
My goal is to help others create better outcomes for our kids. I have treated patients as young as 3 years old and regularly treat in the primary dentition even though I have no special training in treating this age group. Highly motivated mothers can help people like me make treatment happen for their kids when they understand the consequences of failing to act. When it comes to sleep and breathing issues in children, I have seen a direct correlation between early treatment and better long-term outcomes.
James Nestor’s book, Breath, was No. 6 on the New York Times bestseller list and has been published in 32 languages. It has raised public awareness of the importance of nasal breathing and eliminating OSA for people of all ages as a primary health care goal. Helping young children to sleep and breathe well should be part of every pediatric dentist’s skill set. With Nestor’s book and the ADA mandate, the stage has been set for the pediatric dentist to assume the lead in treating the airway.
How can you begin?
With a new focus on sleep and airway health, a number of us are happy to share our experience about when and how to treat kids in the primary or early mixed dentition. Effectively treating this group almost always requires a team of other health care professionals working together. Dr Sheldon goes on to say, “If you identify the problem but can do nothing about it, then the need for identification becomes questionable, so the two cannot be done in isolation.”8 This means pediatric dentists not only need to recognize sleep and breathing problems, they need the skills to actually treat these children. Recognizing the symptoms and identifying the problem are the first steps. There are a number of approaches which can be effective in addressing the airway, and none are a panacea. I’ve had my successes and failures over the past 30 years as I’ve studied this problem. I’ve seen little movement in our profession to fund research to find better approaches. Doing nothing just because there isn’t a perfect answer for every case is not an ethical answer. It is ironic that 100-plus years ago orthodontists were treating these issues before OSA was even given a name, but such treatment disappeared as treatment to align teeth became commonplace.
Hopefully the pediatric dental profession will embrace this public health issue, develop programs to train doctors in current treatment modalities, and fund research to find even better ways. Will the profession take the first step of recognizing more than tooth problems and help dentistry assume a pivotal role in starting children on a lifetime of airway health?
A number of pediatric dentists have already dedicated their practices to treating airway issues. Doing so has transformed their practices, increased their personal satisfaction, and improved the health of their patients. Can you envision you, your practice, and your patients benefitting from your airway awareness? There are people who have already blazed this trail, and we are happy to have you join us on this journey.
 William M. Hang, DDS, MSD, graduated at the top of his class from the University of Illinois College of Dentistry and the University of Minnesota Orthodontic program where he briefly taught orthodontics. He has been in private practice since 1975 and is currently practicing in Agoura Hills, California. Having been traditionally trained, he extracted teeth for crowding and often retracted the teeth. For the past 40 years, however, he has been a pioneer in nonretractive treatments to improve the airway in patients of all ages. He received a Lifetime Achievement Award from the American Academy of Physiological Medicine and Dentistry for his work.
William M. Hang, DDS, MSD, graduated at the top of his class from the University of Illinois College of Dentistry and the University of Minnesota Orthodontic program where he briefly taught orthodontics. He has been in private practice since 1975 and is currently practicing in Agoura Hills, California. Having been traditionally trained, he extracted teeth for crowding and often retracted the teeth. For the past 40 years, however, he has been a pioneer in nonretractive treatments to improve the airway in patients of all ages. He received a Lifetime Achievement Award from the American Academy of Physiological Medicine and Dentistry for his work.
Dr. Hang recently founded OrthO2Health™ to teach and mentor doctors about airway-healthy orthodontic treatments for all ages. His Early Childhood Health-Centered Orthodontic Mentorship™ focuses on treatments for children approximately age 10 and under with an emphasis on treating in the primary dentition. The Hang E.R.R.S.™ (Extraction Retraction Regret Syndrome™) Orthodontic Mentorship addresses treatments for teens and adults to optimize facial balance, TMJ health, and airway. Reversing previous orthodontic retraction, including reopening previous bicuspid extraction spaces or missing lateral incisor spaces and surgery, are also integral parts of this mentorship.
Disclosure: Dr. Hang practices Orthotropics® and has a mentorship in which he teaches other doctors the philosophy and technique of Orthotropics®.
- Harper RM, Kumar R, Ogren JA, Macey PM. Sleep-disordered breathing: effects on brain structure and function. Respir Physiol Neurobiol. 2013 Sep15;188(3):383-391.
- Allen WH, Sedgwick WT. Civics and Health (1909). Boston: Athenaeum Press; 1909.
- Philippe J. Who introduced early treatment to orthodontics? J Dentofacial Anom Orthod 2012;15:107. Available at: https://www.jdao-journal.org/articles/odfen/pdf/
2012/01/odfen2012151p107.pdf Accessed January 3, 2023. - ADA House of Delegates; The Role of Dentistry in the Treatment of Sleep-Related Breathing Disorders. 2017.
- Singh GD, Medina LE, Hang WM. Soft tissue facial changes using Biobloc appliances: geometric morphometrics. Int J of Orthod Milwaukee. 2009;20(2):29-34.
- Singh GD, Garcia-Motta AV, Hang WM. Evaluation of the posterior airway space following Biobloc therapy: geometric morphometrics. 2007;25(2):84-89.
- Boyd KL, Sheldon SH. Sleep disorder breathing: a dental perspective. In: SH Sheldon, MH Kryger, R Ferber, D Gozal, eds. Principles and Practice of Pediatric Sleep Medicine, 2nd edition. London: Elsevier; 2012:275-280.
- Diiulio R. Sleeping Like a Baby: Dr Stephen H. Sheldon’s Pediatric Sleep Medicine Practice. Sleep Review. Nov 2013. https://sleepreviewmag.com/sleep-treatments/therapy-devices/cpap-pap-devices/sleeping-like-a-baby-dr-stephen-h-sheldon-pediatric-sleep-medicine-practice/. Accessed December 20, 2022.
- National Survey of Children’s Health (NSCH) 2016: online and mail survey. https://nschdata.org/browse/survey/. Accessed December 20, 2022.
- Personal communication.
Check out these book reviews on airway health and a healthy lifestyle in our sister publication, Dental Sleep Practice. https://dentalsleeppractice.com/airway-health-as-a-food-choice/
