Using EndoSequence Root Repair Material for more predictable success
Dr. Najia Usman describes the benefits of using EndoSequence BC Pediatric Putty to create a biocompatible and bioinductive antibacterial solution that leads to better patient care for her young patients.

Dr. Najia Usman discussed working with biocompatible and bioactive materials from Brasseler USA
The evolution of my career as a self-proclaimed “Pediatric Endodontist” has been fortuitous. Having graduated from dental school in 1995 and then starting my residency in Portland, Oregon in 2000 meant that I would first be able to see the emergence of modern endodontics as we see it today. The new technology of apex locators, nickel-titanium files, and microscopes made my dental school undergraduate endodontic education seem outdated, but as they say, “You don’t know what you don’t know.” I remember my Chairman Dr. Craig Baumgartner handing me a small photographic film vial with a curious gray powder that I nicknamed “miracle mud.” This was MTA (Mineral Trioxide Aggregate) introduced by Mahmood Torabinejad in 1995 from Loma Linda that was being tested in labs and being given to endodontic residents around the country. It was comprised of tricalcium silicate, tricalcium aluminate, tricalcium oxide, and silicate oxide. Brought to market as ProRoot® by Dentsply, we used to mix it with our local anesthetic to a consistency that allowed the necessary handling properties for the task required. If it was a direct pulp cap, we needed it firm enough to plug into place. If we had a perforation, we needed it to flow and adapt to the defect, and if we needed to pack an open apex (apexification), we needed it to push it the length of the root but still stay put at the apex and not wash out.
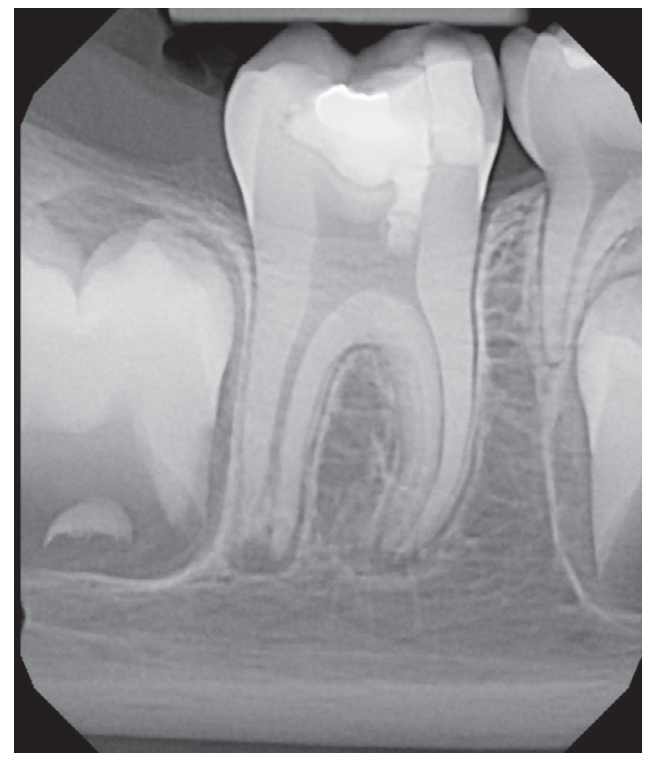
My first “ah-ha” moment came when I saw the closing of a long-standing large sinus tract on my pediatric 8-year-old patient, who after trauma presented with chief complaint of mobility, swelling, and likely a situation that looked hopeless. The biggest challenge with an open apex case is productive disinfection followed by creation of a long-lasting seal. Calcium hydroxide was used as the intracanal medicament between visits. Because it was not radiopaque, it was hard to gauge if it even made critical contact with the periradicular biofilm. I placed a CollaPlug® scaffold gingerly, visualizing with the microscope and then placed the MTA on the CollaPlug pillow taking several radiographs until I felt that I could see the MTA appear to encapsulate the irregularly shaped apex. Despite the visually satisfying post-op radiograph, I would come to see the amazing periapical healing complete with a rejuvenation of the periodontal ligament and concomitant osseous healing.
As we would review the current literature, terms like “biocompatible” and “bioinductive” were words that became associated with this new class of endodontics materials called bioceramics. Originally a purified version of Portland cement, this material was able to demonstrate fibroblast growth on top of its materials. The benefits of this new class of materials were rooted in its alkaline nature and ability to set in the presence of liquid “hydrophilic.” In addition, its excellent sealing properties made it a first choice for almost all complex endodontic applications.
We became very comfortable using it to heal our perforations. We changed from using our “ace in the hole” Super EBA® reinforced IRM in our retropreps following apical surgery to this new material. Despite the benefits though, we were now faced with the challenging handling properties of this material which quickly became a slurried mess when any blood came into our field. I remember Dr. Baumgartner remarking that if we could seal all of our canals with “this stuff” instead of gutta percha, “we would be on to something.”

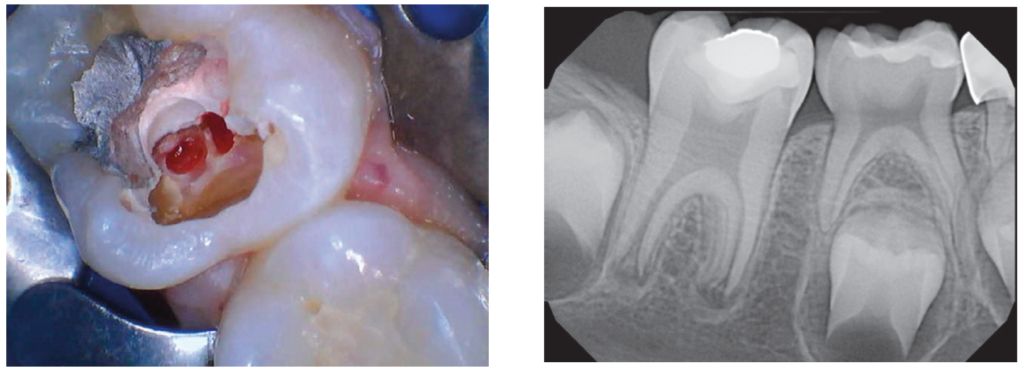
I don’t remember the first time I actually used MTA for an apexogenesis in my private practice, but the circumstances were always the same. I would get a call regarding a fracture to a front tooth with a pulp exposure on an 8-year-old child. If I couldn’t see that child that day, I would instruct my referring dentist to gently cover the pulp exposure with GIC and refer to me ASAP. The protocol required removing a minimum of 2 mm of pulp tissue or until any bleeding stopped. I would use a diamond in a high speed with copious irrigation. Gently disinfecting with chlorohexidene and placing a saturated cotton pellet to assess healthy pulp was critical followed by placing a 2 mm thickness of MTA as a direct pulp cap. In those days, I would place a wet cotton pellet on top of the MTA and seal with Cavit™ per manufacturer’s recommendations. I would then bring the patient back to confirm set of the MTA, absence of symptoms, and do the definitive coronal restoration.
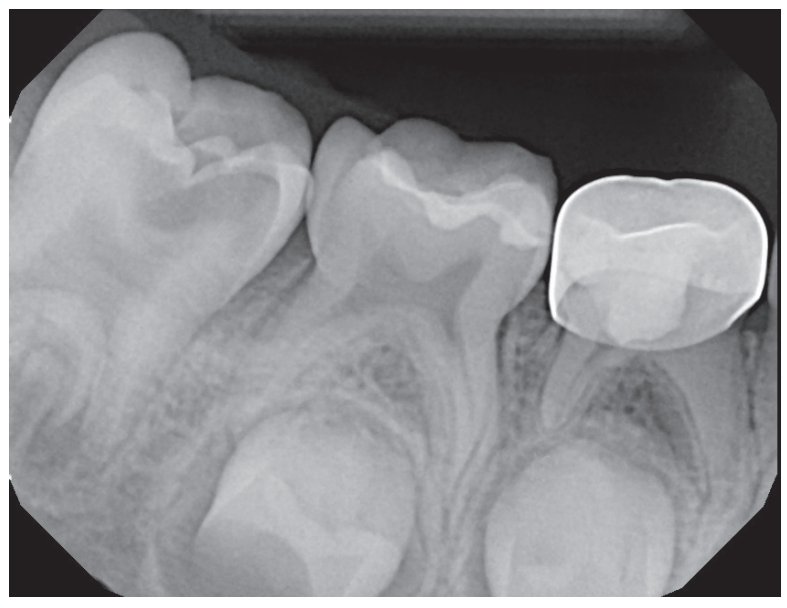
Whether it was a traumatic pulp exposure or a carious pulp exposure on an asymptomatic child with under developed roots, I was seeing consistent success. The patient was remaining asymptomatic because the pulp vitality and health was maintained. I was further rewarded with being able to see that beautiful dentin bridge that developed underneath the MTA protecting that healthy pulp as the root grew in length and closed.
With trauma protocols, we recall these patients quarterly for the first year prepared to intervene with traditional endodontic treatment anytime we see evidence of failure. We then see these patients annually for 5 years, or more often, until I am satisfied that the root growth is complete. Unfortunately, I was starting to see an ugly silver gray halo at the cervical margin as a result of the tooth erupting out of the alveolus as part of the normal growth of the child. All of a sudden, I was faced with another treatment challenge. Now I had to take out my minimalistic composite, remove MTA, and then remove tooth structure to facilitate non-vital bleaching. I remember being very frustrated that we were weakening tooth structure coronally after working so hard to grow the root. I also faced the possibility of damaging the pulp as we had to remove much of that 2 mm MTA cap.
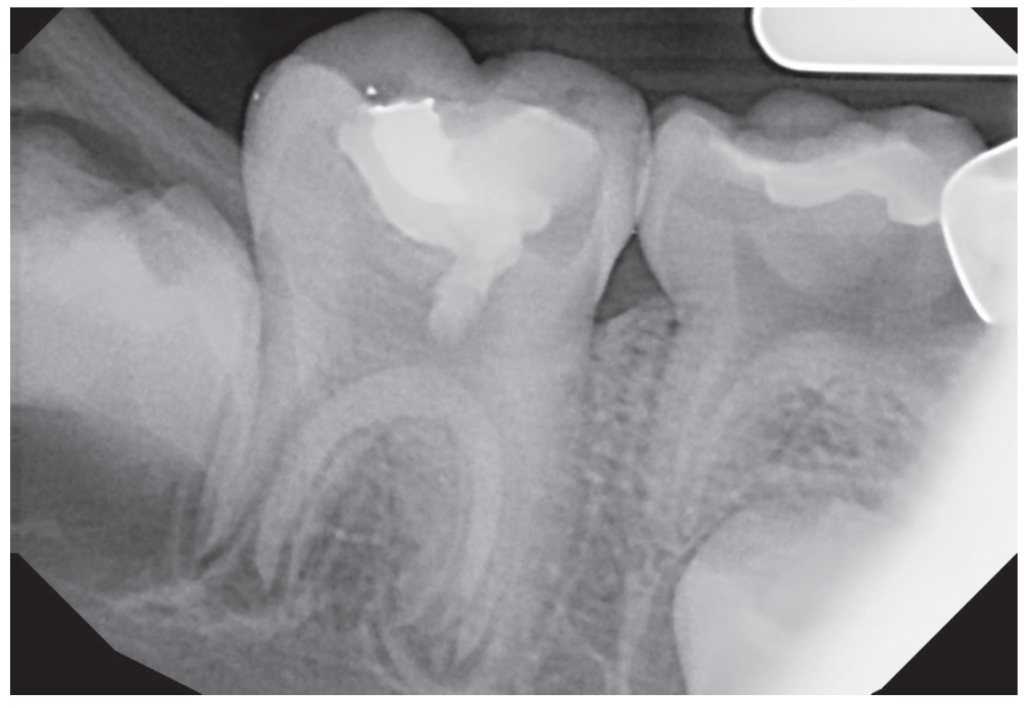
Enter EndoSequence®. I remember my Brasseler rep coming to my office to fulfill my bur order. He asked me if I was familiar with this new bioceramic root repair material in a putty consistency. It has all the desirable qualities of my original MTA but also was the answer to my problems. Now there was a material which had amazing handling properties, did not require pre-mixing, and would bond to dentin because of its hydrophilic properties and very small particle size. A huge benefit was that it would not stain the dentin. At first being a purist, I was reluctant to change because I was so hooked on the benefits of my original MTA. I started using it first in my posterior apexogenesis cases where color was not a concern.
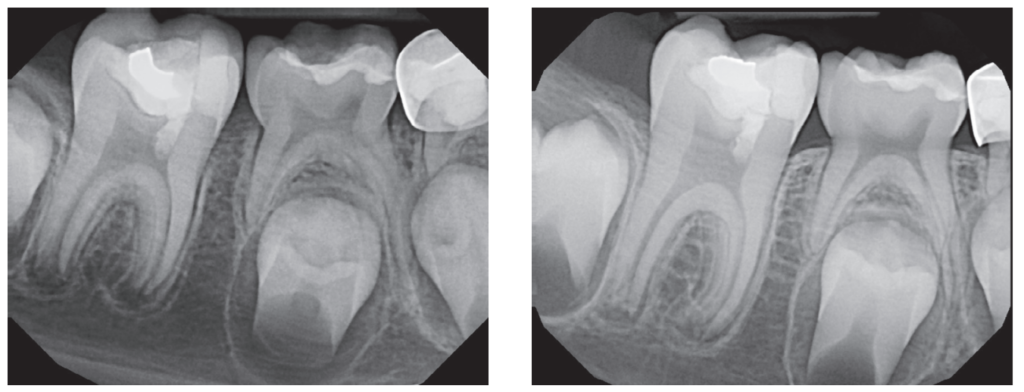
With a published success rate of >95%, Cvec pulpotomies or apexogenesis have become commonplace. Maybe it was my ability to manage children well or the fact that I was able to have consistent results, but my philosophy started to evolve from being reactive to trauma to being proactive. I would convert my referring dentists and pediatric dentists who would send me their “wait and watch” “well-intended” class 4 composites which ultimately became purulent disasters. I have now become the endodontist who lectures around the world about the benefits of placing a bioceramic root repair pulp cap even in a near pulp/dentin (Ellis Class II) exposure with an open apex. Believe me, sometimes when I show periapical radiographs with an open apex and only dentin involvement, I get gasps on the mere suggestion of doing a Cvek. But from my vantage point, vital pulp therapy, which is defined as the art and science of maintaining the vitality of the pulp, is of great value. You see, I meet those patients who have been the recipients of conservative treatment. They are the patients who present with swelling, pain, or discoloration of their teeth. Depending on the age of injury, their apices may be open, and the prognosis even after treatment is far more questionable than if we had controlled the narrative from the beginning.
Armed with this new philosophy rooted in the satisfaction of hundreds of pediatric trauma patients over the last 20 years, I have been lecturing about regenerative endodontics of which vital pulp therapy is part of the treatment spectrum. While I have honed my skills and get consistent results, my mission is to equip pediatric dentists and general dentists to feel just as comfortable doing these procedures. One question I would consistently get from my pediatric residents was the concern about follow-up and the challenge of removing the cotton pellet and placing the definitive restoration. Typically in a pediatric residency, it is unlikely that they will see their patient again. One-year ago, my Brasseler rep provided a solution that has been a game changer in regenerative endodontics as a whole. EndoSequence has now created a liner in blue or white which bonds immediately to the EndoSequence RRM. It is a next-generation bioactive hybrid resin optimized for use with any of the bioceramic sealers and putty materials (BC RRM). What I love about these materials is the ease of dispensing and knowing that their performance is going to assure me of results without all the extra appointments.

For years, pediatric dentists have maintained deciduous teeth in the mouth until natural exfoliation, by performing pulpotomies. The pulpotomy can be defined as the surgical removal or amputation of the coronal pulp of the vital tooth. This step is followed by the placement of a medicament over the intact stump to fix, mummify, or stimulate repair of the remaining radicular pulp. Many materials have been used and investigated and they have differed with regards to biological compatibility, healing capabilities, mutagenicity, cytotoxicity, histological response, and carcinogenic potential. Though there historically have been many treatment approaches, most common is the Formocresol, ZOE pulpotomy.
MTA has shown high success rates clinically and radiographically, and it might offer the best immediate alternative to other medicaments. In the beginning of my career, I spent a small fortune on the original MTA, sold in packets that literally made it more costly than the price of gold. The EndoSequence BC RRM is the perfect material which now comes in cost-effective dispensing that makes it even more desirable. For someone with so many pediactric patients, I’m excited that they have recently launched their EndoSequence BC Pediatric Putty. It has all of the same bioceramic properies as their original BC RRM, including the easy-to-dispense delivery method, but now, it is available in standard and bulk packages at an extremely affordable cost. My hope is that my pediatric colleagues will use the new EndoSequence BC Pediatric Putty coupled with the liner to be able to manage traumatic and carious pulp exposures as well as the vital pulpotomies on deciduous teeth to create an antibacterial solution that is biocompatible and bioinductive, improving our patients’ smiles more predictably.
 Najia Usman, DDS, graduated from SUNY Buffalo in 1995. After completing a 1-year general practice residency at the Cleveland Clinic, she furthered her interest in endodontics by completing a 2-year endodontic residency at Oregon Health and Sciences University, Portland, Oregon in 2002. She was awarded her Diplomate status by the American Board of Endodontics in 2009. Dr. Usman has been in private practice since 2002. She is a clinical associate professor at the Case Western Reserve University School of Dental Medicine where she provides instruction to both dental students and graduate endodontic residents. She is a reviewer for the Journal of Endodontics and serves as chair of the American Association of Endodontics Public and Professional Relations Committee. Though she practices full-scope endodontics, she has cultivated an interest in the endodontic management in trauma, pediatrics, and resorptive lesions. She has organized and lectured in dental trauma symposiums. She has lectured and clinically taught dental students, endodontic and pediatric residents. She has lectured and conducted workshops internationally on topics such as endo-perio, atypical facial pain, regenerative endodontics, and pulpal injuries after orofacial trauma. Her study, “The Influence of Instrument Size on Debridement,” published in the Journal of Endodontics (Feb 2004, vol 30, 110-112) has been cited over 260 times. She is the proud mother of four children ages 18 to 28 and has been married to and shares a private multi-specialty practice with Dr. Faisal Quereshy, OMFS, for 29 years. They reside in Cleveland, Ohio.
Najia Usman, DDS, graduated from SUNY Buffalo in 1995. After completing a 1-year general practice residency at the Cleveland Clinic, she furthered her interest in endodontics by completing a 2-year endodontic residency at Oregon Health and Sciences University, Portland, Oregon in 2002. She was awarded her Diplomate status by the American Board of Endodontics in 2009. Dr. Usman has been in private practice since 2002. She is a clinical associate professor at the Case Western Reserve University School of Dental Medicine where she provides instruction to both dental students and graduate endodontic residents. She is a reviewer for the Journal of Endodontics and serves as chair of the American Association of Endodontics Public and Professional Relations Committee. Though she practices full-scope endodontics, she has cultivated an interest in the endodontic management in trauma, pediatrics, and resorptive lesions. She has organized and lectured in dental trauma symposiums. She has lectured and clinically taught dental students, endodontic and pediatric residents. She has lectured and conducted workshops internationally on topics such as endo-perio, atypical facial pain, regenerative endodontics, and pulpal injuries after orofacial trauma. Her study, “The Influence of Instrument Size on Debridement,” published in the Journal of Endodontics (Feb 2004, vol 30, 110-112) has been cited over 260 times. She is the proud mother of four children ages 18 to 28 and has been married to and shares a private multi-specialty practice with Dr. Faisal Quereshy, OMFS, for 29 years. They reside in Cleveland, Ohio.
Disclsoure: Dr. Najia Usman is a key opinion leader for Brasseler USA.
