LightScalpel 10,600 nm CO2 laser procedures in pediatric patients
A soft tissue CO2 laser can be an important tool in pediatric dentistry for gingivectomies, frenectomies, exposure of impacted teeth, and others — with minimal blood loss and reduced discomfort for the patients.
Martin Kaplan, DMD, and Peter Vitruk, PhD, discuss the safety and efficacy of the CO2 laser
Why 10,600 nm CO2 laser?
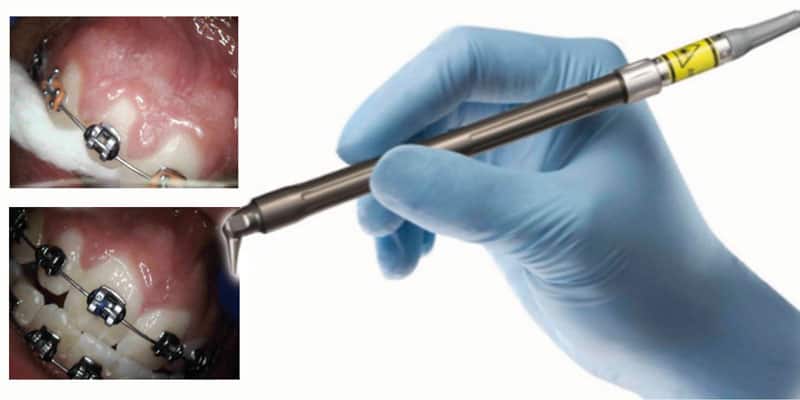
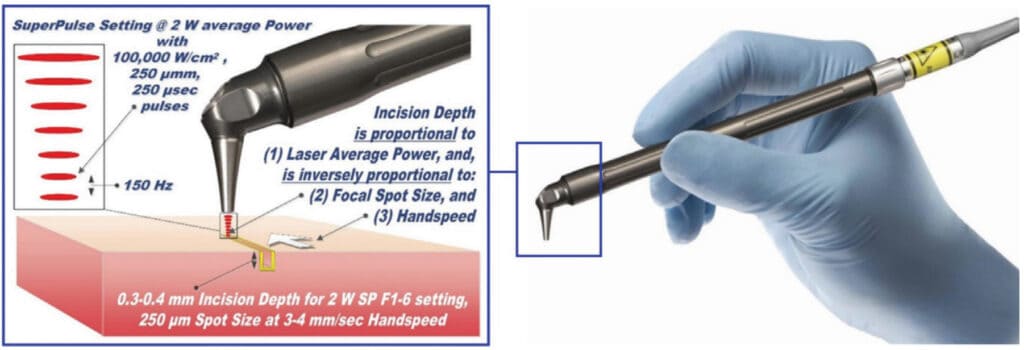
Soft tissue surgical lasers have many advantages over traditional scalpel surgery, cryosurgery, and electrosurgery. However, not all lasers are equally efficient at both cutting the soft tissue and coagulating and hemostasis because light absorption in the soft tissue varies with wavelength.1-3 Some dental laser wavelengths (around 1,000 nm such as diodes and Nd:YAG) are efficient coagulators but inefficient scalpels since they are poorly absorbed by the soft tissue. Other dental laser wavelengths (around 3,000 nm such as Erbium lasers) are well absorbed by the water-rich soft tissue and are great at cutting but are not as efficient at coagulating and hemostasis. The 10,600 nm CO2 laser’s coagulation depth closely matches blood capillary diameters.2 The radiant energy of the CO2 laser is used directly to photo-thermally vaporize (cut, incise, ablate) and, at the same time, photo-thermally coagulate the soft tissues. The CO2 laser is a “What You See Is What You Get” surgical soft tissue laser with minimal collateral thermal effects that are sufficient for sealing blood vessels, lymphatics, and nerve endings; the surface bacteria are efficiently destroyed4 on incision/ablation margins. The modern flexible fiber CO2 lasers from LightScalpel, Inc. (Bothell, Washington) use scalpel-like ergonomic autoclavable handpiece (Figure 1) for (a) cutting, (b) ablation, and (c) photo-thermal hemostasis and coagulation. An important built-in safety feature is a sub-millimeter superficial depth of laser beam incision5 at low power settings (see Figure 1), which makes the CO2 laser a gentler and more forgiving tissue vaporization instrument in comparison with a scalpel, electro-surge, or hot glass diode surgery. Also quick switch from cutting to coagulation mode is enabled by simply defocusing the beam (laser beam fluence dropping below the ablation threshold of 3 Joules/cm2).2 For the CO2 laser, its excellent coagulation efficiency is due to the close match between the sub-100 µm photo-thermal coagulation depth2 and the oral soft tissue blood capillary diameters of approximately 20-40 µm.6
Minimized bleeding for enhanced visibility and precision
The enhanced hemostatic ability and precision of the CO2 laser is especially valuable in visible (esthetic) zones. The CO2 laser surgical removal of the tissue presented in Figures 2-8 illustrates excellent coagulation and hemostasis during soft tissue ablation.2

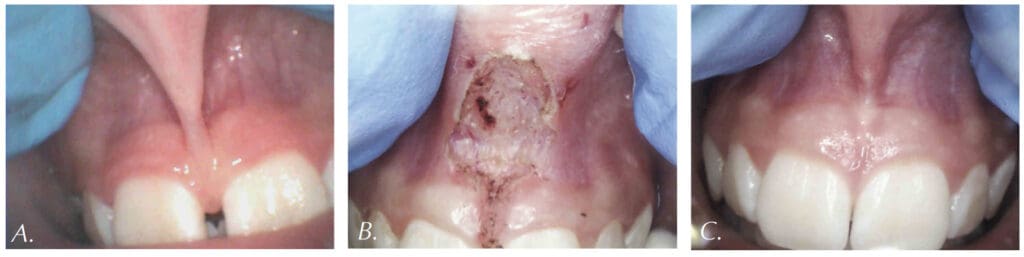
For example, Figures 2A-2C show the use of LightScalpel LS-1005 CO2 laser (2 watts SuperPulse Repeat Mode with F1-6 through F1-8 settings) for soft-tissue crown lengthening of the maxillary incisors and for labial frenum revision. Both procedures were performed during the same visit while the patient received local anesthesia. No sutures were placed. Figure 2 presents the self-correction of a rotated tooth No. 9 after frenum revision. Laser frenectomies in Figure 3 resulted in spontaneous closure of midline diastemas.
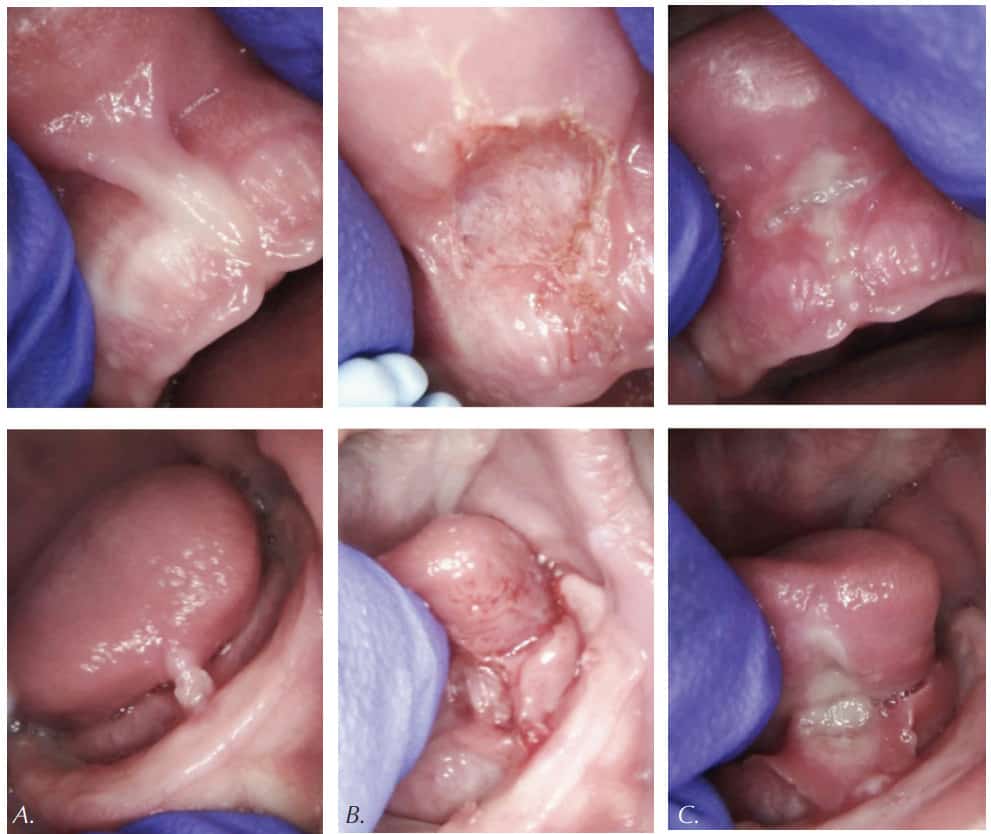
The CO2 laser accuracy is especially important for highly vascularized areas. For example, the 14-year-old patient in Figure 4 had a CO2 laser lingual frenectomy performed during which a sublingual vein was exposed and coagulated (sealed) with defocused laser beam. As a result, no sutures were needed, and the surgical wound was left to heal by secondary intention.

Figure 5 summarizes the case of a 4-week-old bottle-fed baby, born at 8 lbs. 6 oz., not able to breastfeed and failing to gain weight during first 4 weeks of her life. The baby exhibited fussiness and gassiness post feeds and choked often during feeds. Oral exam revealed “wrinkled-looking” gingiva (possible sign of dehydration) and a restricted lip frenum that was corded, thick and tight, and an anterior, tight, calloused and short tongue-frenum causing a significant tongue mobility reduction (Figure 5A). Figure 5B illustrates the clean blood-free laser ablation. Release of tension and ability to flange the lip is now evident. At the 7-day follow-up (Figure 5C), the mother reported feeding times were more efficient, and baby’s weight gain was 1 lb. 11 oz. in the 7 days since surgery. At the 3-month follow-up, the baby now weighed 20 lbs. (9072 gm). There were no more feeding symptoms, and the baby was doing well. Unfortunately, the baby never returned to breastfeeding.
The CO2 laser is also an excellent tool to remove the excess soft tissue. Many pediatric patients require banding of molars, but an overlying operculum gets in the way of placing appliances on these teeth. Figure 6 presents the LightScalpel LS-1005 CO2 laser operculectomy (3 watts SuperPulse Repeat Mode F1-7) prior to band placement. Tissue hemostasis allows for banding to happen immediately after the CO2 laser procedure — bands were seated shortly after operculectomy was performed, in the same visit.

CO2 laser use in the presence of orthodontia hardware
Figures 7-8 demonstrate a completely bloodless CO2 laser gingivectomy around the mandibular incisors in the orthodontic patient. CO2 laser gingivectomies, such as the ones presented in Figures 7-8, help improving the esthetics and oral health; they also allow for more ideal bracket placement and quicker treatment with less appointments.

Gaining access to an impacted tooth or teeth is often necessary in order to place orthodontic braces. With conventional scalpel surgery, many problems occur when placing brackets, such as sutures breaking before brackets are bonded. Brackets will not bond properly if enamel is wet due to bleeding. Clean, bloodless enamel is necessary for enamel acid etching and bonding of the composite resin. Using the CO2 laser to expose an impacted tooth produces a dry surgical field, thus creating conditions required for immediate bracket bonding. The CO2 laser-assisted cuspid exposure procedure is shown in Figure 9. This quick CO2 laser treatment allows access for bracket placement, saving the patient months of waiting for the tooth to erupt on its own. The CO2 laser provides a clean, nonbleeding border. The CO2 laser straight and angled handpieces, illustrated in Figure 1, permit a convenient reach into areas that may be obstructed by braces. Once an impacted tooth is exposed by laser ablation, the bloodless surgical field is ready for the next step. The orthodontic traction hook can be bonded to the exposed enamel immediately after ablation during the same visit saving time for both the patient and clinician.

Tissue healing
Studies have shown that there is a diminished risk of scarring and wound contraction associated with CO2 laser surgery.9 Laser-induced wounds heal with greater fibroblast proliferation, with young fibroblasts actively producing collagen. Laser wounds also have been reported to contain smaller amounts of myofibroblasts (cells responsible for wound contraction), compared to scalpel wounds.9 Secondary intention healing and lack of scarring are especially important for treating lesions located in esthetic/visible zones.

Reduced postoperative pain and discomfort
Patients report less postoperative pain and discomfort with laser surgery.9 The healing process associated with CO2 laser surgery is enhanced and less painful than with cryosurgery or electrosurgery.9
Summary
The many uses for a soft tissue CO2 laser in pediatric dentistry and orthodontics — e.g., gingivectomies, frenectomies, exposure of impacted teeth, and others — feature minimal blood loss and reduced discomfort for the patients. In comparison with other dental laser wavelengths (circa 1,000 nm for diode and Nd:YAG lasers and circa 3,000 nm for erbium lasers), the CO2 laser wavelength exhibits the least absorption rate by the stainless steel orthodontia hardware and the optimum coagulation depth closely matching gingival blood vessel diameters. The CO2 laser ablation depth can be controlled to a few tenths of a millimeter, which characterizes this wavelength as a safe and gentle soft tissue removal tool, while the sub-100 µm coagulation depth (significantly better than hot glass diodes)2,5 allows for enhanced, scar-free healing of highly vascular oral tissues secondary intention.5,9 The accuracy and precision of CO2 laser surgery are increased by the visibility of the surgical field not being obscured by bleeding.
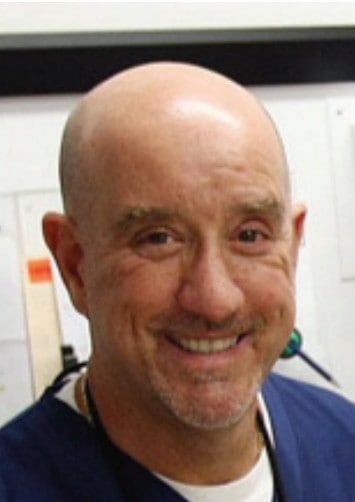 Martin Kaplan, DMD, completed his undergraduate degree at the University of Massachusetts and then attended Tufts University School of Dental Medicine. After earning his DMD degree, he completed a pediatric residency at Montefiore Hospital in New York. He is a member of American Academy of Pediatric Dentistry, Massachusetts Academy of Pediatric Dentistry, American Dental Association, Massachusetts Dental Society, Academy of Sports Dentistry, Massachusetts Breastfeeding Coalition, and Breastfeeding USA. When not practicing dentistry, Dr. Kaplan enjoys Ballroom Dancing and Karate in his spare time.
Martin Kaplan, DMD, completed his undergraduate degree at the University of Massachusetts and then attended Tufts University School of Dental Medicine. After earning his DMD degree, he completed a pediatric residency at Montefiore Hospital in New York. He is a member of American Academy of Pediatric Dentistry, Massachusetts Academy of Pediatric Dentistry, American Dental Association, Massachusetts Dental Society, Academy of Sports Dentistry, Massachusetts Breastfeeding Coalition, and Breastfeeding USA. When not practicing dentistry, Dr. Kaplan enjoys Ballroom Dancing and Karate in his spare time.
 Peter Vitruk, PhD, is a founder of the American Laser Study Club and LightScalpel, Inc. in Bothell, Washington and a member of The Institute of Physics, London, UK. Dr. Vitruk can be reached at 1-866-589-2722, or pvitruk@lightscalpel.com.
Peter Vitruk, PhD, is a founder of the American Laser Study Club and LightScalpel, Inc. in Bothell, Washington and a member of The Institute of Physics, London, UK. Dr. Vitruk can be reached at 1-866-589-2722, or pvitruk@lightscalpel.com.
- Jacques SL. Optical properties of biological tissues: a review. Phys Med Biol. 2013;58(11):37-61.
- Vitruk P. Oral Soft Tissue Laser Ablative & Coagulative Efficiencies Spectra. Implant Practice US. 2014;7(6):22-27.
- Vogel A, Venugopalan V. Mechanisms of pulsed laser ablation of biological tissues. Chem Rev. 2003;103(2):577-644.
- Cobb C, Vitruk P. Effectiveness of a Super Pulsed CO2 Laser for Removal of Biofilm from Three Different Types of Implant Surfaces: An In Vitro Study. Implant Practice US. 2015;8(3):14-20.
- Riek C, Vitruk P. Incision and Coagulation/Hemostasis Depth Control During CO2 Laser Lingual Frenectomy. Dent Sleep Practice. Spring 2018:32-38.
- Yoshida S, Noguchi K, Imura K, Miwa Y, Sunohara M, Sato I. A morphological study of the blood vessels associated with periodontal probing depth in human gingival tissue. Okajimas Folia Anat Jpn. 2011;88(3):103-109.
- Gama SK, De Araujo TM, Pinheiro AL. Benefits of the use of the CO2 laser in orthodontics. Lasers Med Sci. 2008; 23(4):459-465.
- Wolfe WL, Zissis GJ. The Infrared Handbook. Office of Naval Research: Washington DC, 1985: 7-81.
- Glazkova A, Vitruk P. CO2 Laser Surgery Post-Operative Pain and Healing: A Partial Literature Review. Dent Sleep Practice. Winter 2019:28-34.
A CO2 laser can also help in implant practices. Read about how this tool can alleviate the late implant failure linked to tissue tension in our sister publication Implant Practice US. https://implantpracticeus.com/the-10-6-%C2%B5m-superpulse-co2-laser-may-alleviate-the-late-implant-failure-linked-to-tissue-tension/
