New possibilities in aligner therapy
Drs. Steven R. Olmos, Kristina Wolf, and Emily B. Levy tackle craniofacial and respiratory issues on younger patients with a new type of clear aligner therapy.
Drs. Steven R. Olmos, Kristina Wolf, and Emily B. Levy discuss craniofacial and respiratory dysfunction therapy for all ages
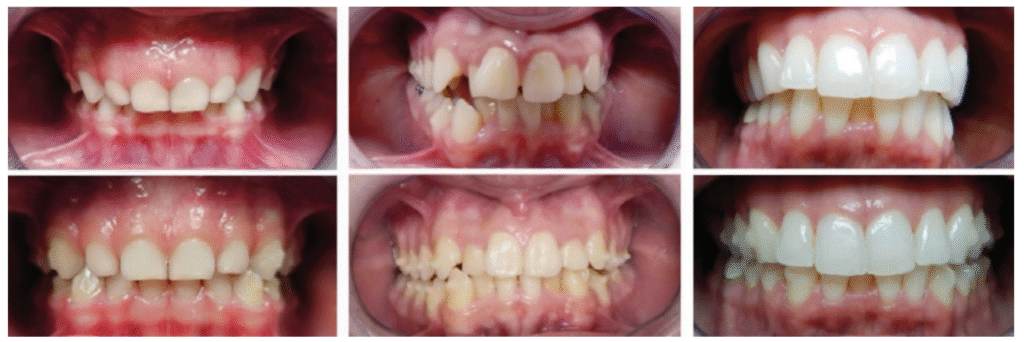
The importance of proper respiration, temporomandibular joint disorder (TMD), facial pain, malocclusion, and posture have been covered in the orthodontic literature. Aligner therapy has an increasing presence as a delivery choice of patients and clinicians. This article compares various systems for arch development and aligner mechanisms and how they can improve whole body function — specifically, in combination with removable functional maxillary arch development devices for adults and children.
Non-surgical craniofacial changes and resolution of chronic TMD and respiratory pathology (mouth breathing and obstructive sleep apnea [OSA]) of a late-20s adult case study was published in a previous article for this journal.1 A case study of pediatric severe apnea/obesity/TMD/headache was resolved through functional development of the maxilla and was also published in this journal.2 These cases required fixed and removable functional development orthopedic devices to achieve these results. We investigate the possibility of replacing these traditional techniques with 3D-printed removable functional development devices in combination with aligner therapy and photobiomodulation (laser).
The relationships between improper respiration (sleep disordered breathing, mouth breathing, nasal obstruction) and malocclusion are well known.3,4 These conditions are comorbid with maxillary deficiency and position to cranial base. This is demonstrated by the incidence of children with Down syndrome who have pediatric obstructive sleep apnea (POSA) after tonsil and adenoid (T and A) surgery at 65%-73%.5,6,7,8
Maxillary insufficiency results in nasal pathology which can result in mouth breathing, snoring, aggravation of obstructive sleep apnea, and forward head posture. This is supported by studies demonstrating that maxillary development can improve OSA and nasal function by increasing volume.9,10 It has been shown that maxillary expansion can shrink T and A and increase the width of the internal nasal valve (which is the first point of entry of air into the nose).11,12 Nasal valve compromise (narrowing of the internal nasal valve) has been found to result in a 7-times greater chance of TM joint capsulitis and facial and cervical myositis, via mouth breathing, when compared to other nasal obstructions.13 Maxillary expansion has been demonstrated to reduce mouth breathing and upright head posture.14,15 Forward head posture is a compensatory mechanism in order to improve respiratory muscle function in children with mouth breathing, which results in submaximal exercise performance.16
Comparisons to other orthodontic aligner and functional orthodontic systems
In recent years, there has been an increase in the use of clear or “invisible” aligner systems in adult populations in lieu of traditional orthodontic treatments. The use of clear aligners provides a more esthetic and comfortable treatment option and allows for better oral hygiene. Clear aligners have commonly been used in simpler orthodontic cases; however, over the years, clear aligners have been utilized in more complex cases of malocclusion.
In 1997, Align Technologies brought to market the original aligner product that set the standard for clear aligner therapy. With this application of light and constant forces by use of the aligners, teeth can move biomechanically. However, when assessing and addressing any root cause dysfunctions, such as muscle function, tongue position, or more completely treating the entire craniofacial complex, Invisalign™ and other clear aligners have significant limitations to their functionality. Furthermore, because of the simplistic nature of the biomechanics and dento-alveolar tooth movement, the complexity of cases able to be treated with Invisalign™ is diminished, allowing treatment of simple and moderate cases of malocclusion, with severe limitations in complex malocclusions.17
More recently, focus has been given to proper functionality of the craniofacial complex and the use of prefabricated myofunctional appliances (PMAs).17 PMAs are soft, elastomeric, removable orthodontic appliances which provide shields around the upper and lower dentition in order to correct malocclusions. These appliances, such as Myobrace®, are widely advocated for use in correcting more complex malocclusions with use for 10 hours per day. PMAs focus on functionality, and they are designed to correct oral habits such as tongue thrust, as well as improve proper, functional nasal breathing. Myofunctional therapy has been shown to reduce AHI by 50% in adults and 62% in children.18
Combining clear aligners with functional appliances
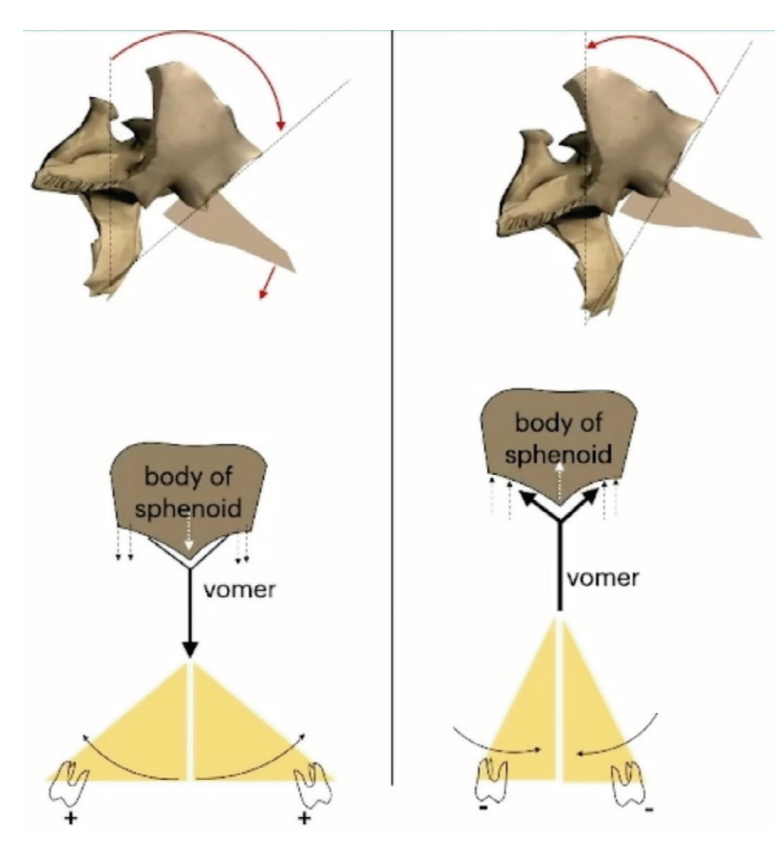
Traditional orthodontic treatment has been based on light and constant forces; however, nature adapts the morphology with forces that are cyclical. When attempting to create 3-dimensional changes to the cranium, and therefore the dentition as well, providers need to look beyond dento-alveolar forces and observe the adaptation of the sutures of the skull. Cyclical forces are commonly seen in the human body. Mastication, breathing, cardiac function, and cerebrospinal fluid (CSF) flow are all cyclical forces. When these forces become dysfunctional, there will be asymmetry of the face, posture, and occlusion. Cyclical forces will change the morphology of the bone. During treatment, the goal must be to not only attempt tooth or dental movements, but cranial movements as well (Figure 1).
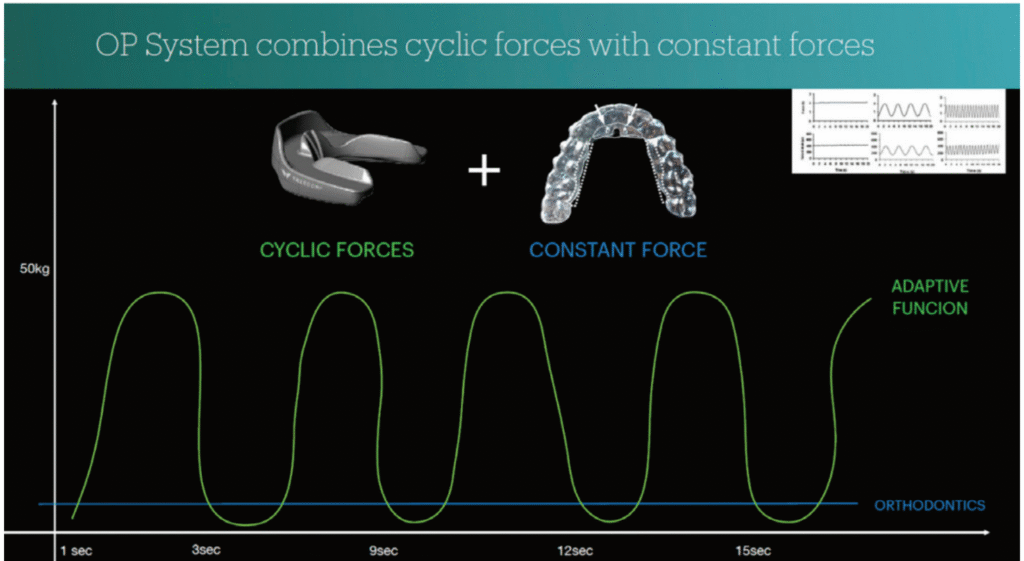
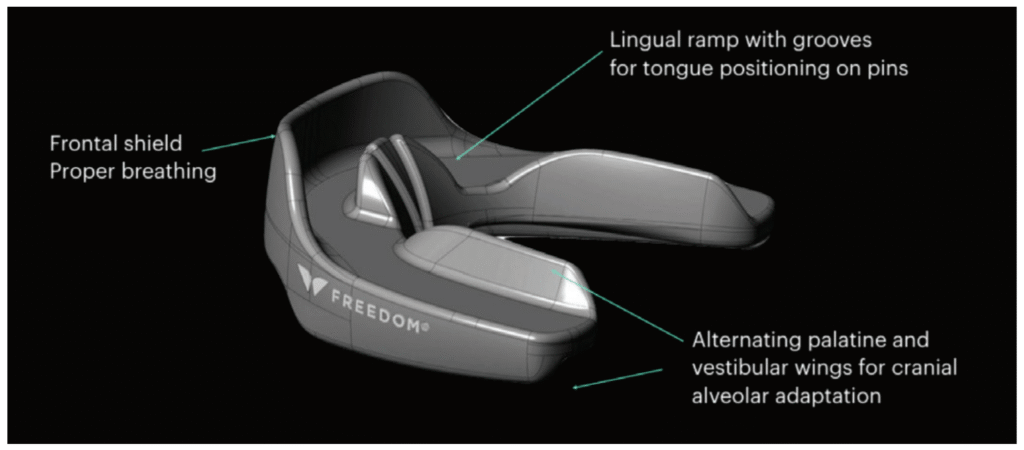
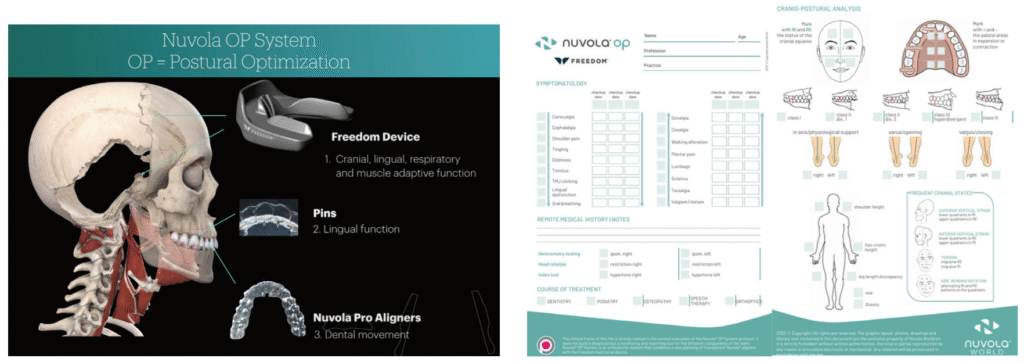
The Nuvola® OP system, a new orthodontic protocol, has been in existence since 2019. This system combines PMAs with specifically designed aligners in an innovative way. This is the first aligner system designed to be used alongside a myofunctional device. With the combination of these therapies, there is an enhanced biomechanical action, combining the light, constant forces of orthodontic aligners with the cyclical forces needed for proper function by chewing of the myofunctional device, the Freedom™ appliance (Figure 2). The combination of these therapies allows for functional correction along with mechanical tooth movement.
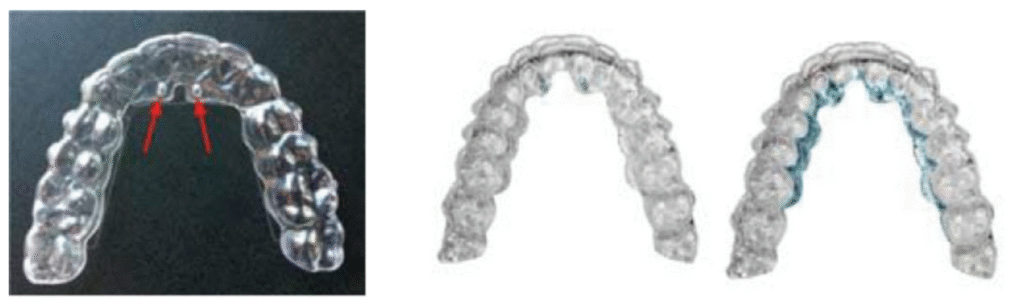
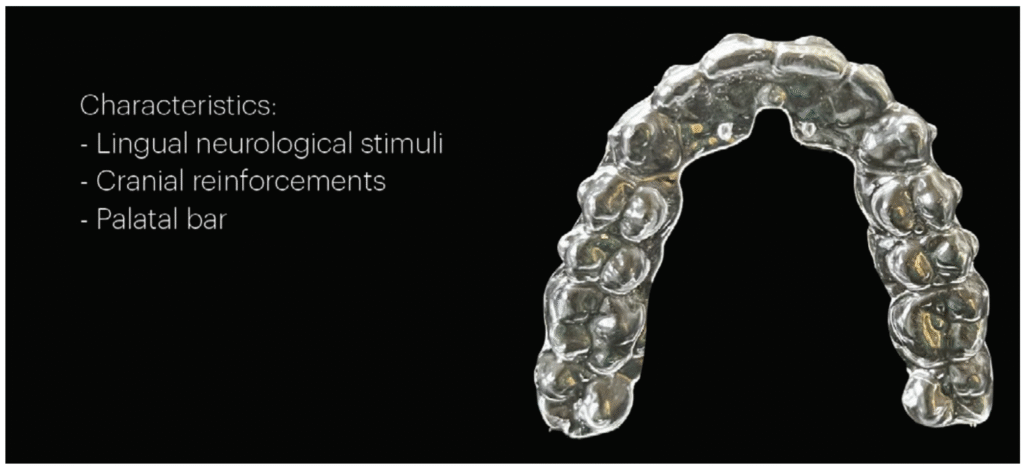
These components differ from other systems in a variety of ways. The Nuvola Pro™ clear aligners have palatal reinforcement areas (Figures 3 and 4). Adequate pressure applied by use of the Freedom™ appliance allows a slight deformation of these palatal areas by its sutures (Figure 5). These reinforced areas have slightly more coverage along the palate, and have improved biomechanics, which allows for a multitude of treatment possibilities depending on a patient’s cranial pattern, cranial dysfunction, and malocclusion. The Nuvola Pro™ aligner also includes lingual pins in order to attract the tongue and to activate muscle and tongue training (Figure 3). This guides the tongue to the proper position and allows for correction of functional concerns which are commonly missed by traditional aligners.
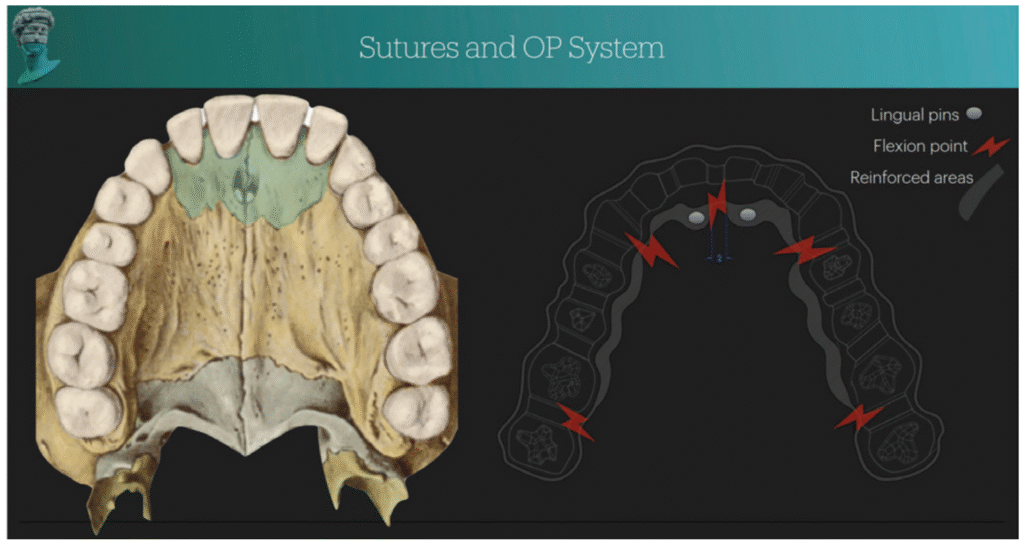
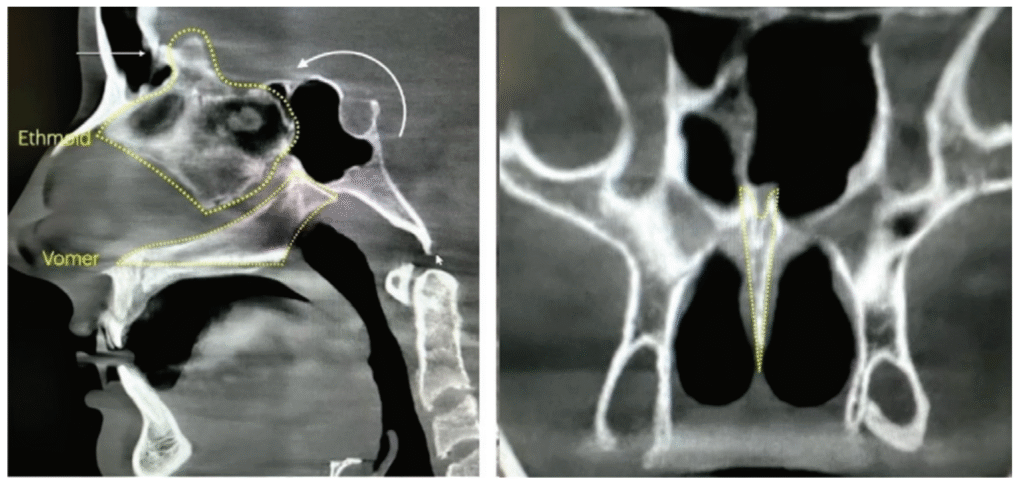
The specially designed Freedom™ appliance (Figure 2) offers three distinct flexion areas (Figure 5) and is to be used in conjunction with the Nuvola Pro™ aligners. In adults, aligners are used 20 hours per day. Patients are instructed to clench for 30 minutes per day on the Freedom™ appliance with the aligners in place. The Freedom™ appliance is specially designed to be used with this type of aligner and helps with recruitment of muscles to transmit adaptive forces to the whole of the craniofacial complex. The use of the Freedom™ with the Nuvola Pro™ aligners activates muscles, such as the masseters, temporalis, and pterygoids, through chewing motions. The specific flexion areas allow correction of the palate and are designed to allow guided, cyclic deformation of the aligners. This allows the cyclic force system to be activated, which is the driving force needed at the sutural level (Figure 1). The maxillary spine (anterior nasal spine) is engaged by the action of the lingual ramp of the Freedom™ appliance and the lingual pins of the aligners. This results in a piston action on the vomer which engages the sphenoid (cranial base) and is the mechanism of cranial remodeling (Figures 6 and 7). The frontal shield of the Freedom™ device, acting as a PMA, activates the orbicularis oris muscle promoting lip competency and proper nasal breathing. This system, therefore, combines the constant and light forces of traditional orthodontics (via the Nuvola Pro™ aligners) with stronger cyclical forces by contraction of the muscles of mastication and adaptation of cranial sutures (via the Freedom™ appliance) (Figure 8).19
A comprehensive examination is recommended for all patients with malocclusion and functional deficits. Nuvola® has a custom medical information form to be used during an exam, including a posture evaluation (Figure 9).
Pediatrics
When treating the pediatric patient population, early intervention is especially critical to redirect abnormal craniofacial growth, especially because the mandible and maxilla have both reached approximately 85% of their adult size by 5 years of age.20,21 Maxillary insufficiency contributes to mouth breathing, snoring, obstructive sleep apnea (OSA), and forward head posture. Breathing disorders can be functional (with regards to mouth breathing) or sleep-related, but all dysfunctional breathing cases are underdeveloped when compared to cases of nasal respiration.
A comprehensive exam for children is required prior to treatment, including intraoral photographs, postural photos, cephalometric radiography and tracing of the skull, CBCT scan, and intraoral scan impressions. Lingual frenulum function should also be evaluated, as literature shows a relationship between a short lingual frenulum and maxillary hypoplasia, as well as increased risk for the onset of OSA.22,23 A referral for a sleep evaluation may be necessary to diagnose an underlying breathing disorder.
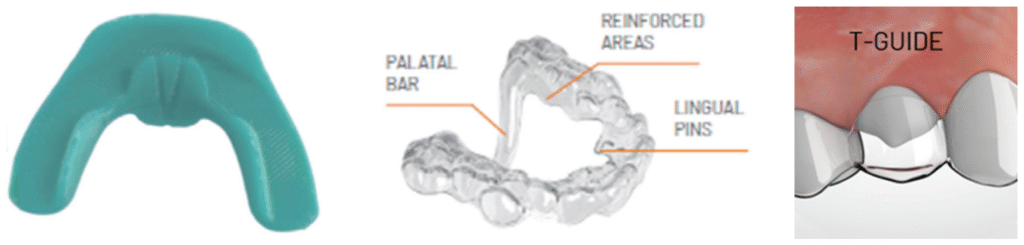
The Nuvola Junior™ system incorporates Nuvola Pro™ aligners and the Freedom Mini™ device to develop the maxilla and the cranium for optimal function in children as young as 4 (or younger with compliance). The Freedom Mini™, much like the previously discussed Freedom™, incorporates piezoelectric forces of mastication, encourages lip seal and nasal breathing, directs forces to create cyclic movements of the cranium and maxilla, and is minimally invasive (Figure 10). Balancing orofacial forces creates a more optimal growth pattern by allowing skeletal adaptations of the skull through myofunctional stimuli.22 Nuvola Junior™ aligners can be fabricated with a palatal bar to facilitate increased expansion, as well as T-guides to guide eruption of permanent dentition (Figures 11 and 12). Nuvola® can also be utilized to upright, torque, or extrude teeth.
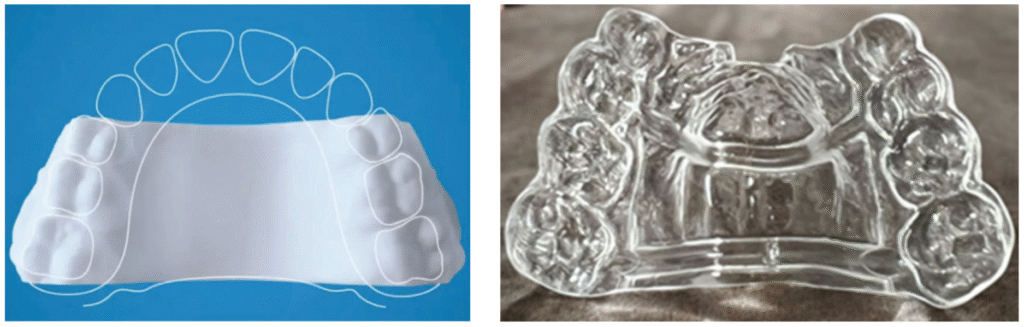
Invisalign™ has introduced a 3D-printed palatal expander intended for use in 6–11-year-olds (Figure 13). It acts as primarily linear, transverse expansion, without development of the cranium or the premaxilla.24 When treating pediatric breathing disorders, the entirety of the maxilla must change. The Nuvola Junior™ system, like the Nuvola OP™ system, allows recovery of transversality and encourages pre-maxillary development, changing the maxilla in all dimensions by using the sphenoid and vomer to stimulate other cranial bones.19
A new Nuvola® appliance, the Sprint Arch-Conformer, will be available soon (Figure 14). It is a sequential thermoformed aligner and will have a certain degree of flexibility in order to take advantage of the natural adaptive capacity of all of the sutures of the palate, as well as development of the premaxilla. This appliance will allow for more rapid growth of the maxilla and cranium using a double palatal bar. In conjunction with the Freedom™ device, it will combine cyclic and continuous forces to avoid the cranial strain that is seen in traditional RPE devices.
Daytime wear of aligners in children is age-dependent, ranging from 2 hours to all-day. All ages wear the aligners at night. Children perform clenching on the Freedom Mini™ for 30 minutes per day in conjunction with the Nuvola Pro™ aligners in order to improve muscle tone, tongue posture, deglutition, and respiratory habits. In case reports, all objective assessments moved towards improvement after treatment, improving arch dimensions, creating expansion, and correcting cervical hyper-lordosis.22
Nuvola® internal case reports also show a decrease in soft palate length and improved lingual posture, both of which are known to be increased risk factors for OSA.22,25 Maxillary development leads to reduction of size of tonsils and adenoids, increase in size of the internal nasal valve, and improved flow rate of air through the nose.10,11,12 Coupling development and function during treatment allows for less orthodontic relapse than in traditional methods, regardless of fixed retention, especially in the maxilla.26,27

With all Nuvola® OP and Nuvola Junior™ devices, laser therapy can be used to facilitate more efficient craniofacial changes and tooth movement. Photobiomodulation (laser) therapy has been shown to decrease time spent in aligners and decrease pain associated with orthopedics and orthodontics.28,29 The MLS and M Hi-D (BioResearch) and NdYag (DEKA) lasers facilitate osteoblast and osteoclast activity on the maxillary sutures and decrease inflammation (Figure 15).
Future studies will determine efficacy of the Nuvola® OP/Nuvola Junior™ system to treat pediatric OSA. If proved to be efficacious for treatment of sleep breathing disorders, the Nuvola Junior™ system can begin treatment on even younger patients to facilitate craniofacial development and habitual nasal breathing, the only valid endpoint of treating pediatric OSA.30
 Steven R. Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO, is Founder and Director of Education at TMJ and Sleep Therapy Centres International. www.tmjtherapycentre.com
Steven R. Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO, is Founder and Director of Education at TMJ and Sleep Therapy Centres International. www.tmjtherapycentre.com
Kristina Wolf, MS, DMD, DABDSM, is from the TMJ and Sleep Therapy Centre of Cleveland, and is a Lecturer, Mini-Residency, TMJ and Sleep Therapy Centres International.
Emily B. Levy, DDS, FAACP, FOM, is from the TMJ and Sleep Therapy Centre of New Orleans, and is a Lecturer, Pediatric OSA Mini-Residency, TMJ and Sleep Therapy Centres International.
Disclosure: BioResearch and Nuvola are sponsors of T & S Therapy Centre International, LLC courses.
- Olmos SR. Improving quality of life and faces nonsurgically. Orthodontic Practice US. 2017;8(3):36-43.
- Olmos SR. Pediatric severe apnea/obesity/TMD/headache — Class III. Orthodontic Practice US. 2016;7(3): 20-24.
- Aroucha Lyra MC, Aguiar D, Paiva M, Arnaud M, Filho AA, Rosenblatt A, Thérèse Innes NP, Heimer MV. Prevalence of sleep-disordered breathing and associations with malocclusion in children. J Clin Sleep Med. 2020 Jul 15;16(7):1007-1012. doi: 10.5664/jcsm.8370.
- Huynh NT, Morton PD, Rompré PH, Papadakis A, Remise C. Associations between sleep-disordered breathing symptoms and facial and dental morphometry, assessed with screening examinations. Am J Orthod Dentofacial Orthop. 2011 Dec;140(6):762-770. doi: 10.1016/j.ajodo.2011.03.023.
- Shott SR, Amin R, Chini B, Heubi C, Hotze S, Akers R. Obstructive sleep apnea: Should all children with Down syndrome be tested? Arch Otolaryngol Head Neck Surg. 2006 Apr;132(4):432-436. doi: 10.1001/archotol.132.4.432.
- Maris M, Verhulst S, Wojciechowski M, Van de Heyning P, Boudewyns A. Prevalence of obstructive sleep apnea in children with down syndrome. March 2016;39:699–704.
- Hill CM, Evans HJ, Elphick H, Farquhar M, Pickering RM, Kingshott R, Martin J, Reynolds J, Joyce A, Rush C, Gavlak JC, Gringras P. Prevalence and predictors of obstructive sleep apnoea in young children with Down syndrome. Sleep Med. 2016 Nov-Dec;27-28:99-106. doi: 10.1016/j.sleep.2016.10.001. Epub 2016 Oct 22. Erratum in: Sleep Med. 2017 Jun;34:249. doi: 10.1016/j.sleep.2017.02.003.
- Dyken ME, Lin-Dyken DC, Poulton S, Zimmerman MB, Sedars E. Prospective polysomnographic analysis of obstructive sleep apnea in down syndrome. Arch Pediatr Adolesc Med. 2003 Jul;157(7):655-660. doi: 10.1001/archpedi.157.7.655.
- Cistulli PA, Palmisano RG, Poole MD. Treatment of obstructive sleep apnea syndrome by rapid maxillary expansion. 1998 Dec 15;21(8):831-835. doi: 10.1093/sleep/21.8.831.
- Motro M, Schauseil M, Ludwig B, Zorkun B, Mainusch S, Ateş M, Küçükkeleş N, Korbmacher-Steiner H. Rapid-maxillary-expansion induced rhinological effects: a retrospective multicenter study. Eur Arch Otorhinolaryngol. 2016 Mar;273(3):679-687. doi: 10.1007/s00405-015-3584-y. Epub 2015 Apr 3.
- Yoon A, Abdelwahab M, Bockow R, Vakili A, Lovell K, Chang I, Ganguly R, Liu SY, Kushida C, Hong C. Impact of rapid palatal expansion on the size of adenoids and tonsils in children. Sleep Med. 2022 Apr;92:96-102. doi: 10.1016/j.sleep.2022.02.011. Epub 2022 Feb 19.
- Yoon A, Abdelwahab M, Liu S, Oh J, Suh H, Trieu M, Kang K, Silva D. Impact of rapid palatal expansion on the internal nasal valve and obstructive nasal symptoms in children. Sleep Breath. 2021 Jun;25(2):1019-1027. doi: 10.1007/s11325-020-02140-y. Epub 2020 Jul 9.
- Olmos SR. Nasal airway obstruction and orofacial pain: a multicenter retrospective analysis. Gen Dent. 2022 Nov-Dec;70(6):28-33.
- Tecco S, Festa F, Tete S, Longhi V, D’Attilio M. Changes in head posture after rapid maxillary expansion in mouth-breathing girls: a controlled study. Angle Orthod. 2005 Mar;75(2):171-176. doi: 10.1043/0003-3219(2005)075<0167:CIHPAR>2.0.CO;2.
- McGuinness NJ, McDonald JP. Changes in natural head position observed immediately and one year after rapid maxillary expansion. Eur J Orthod. 2006 Apr;28(2):126-34. doi: 10.1093/ejo/cji064. Epub 2005 Sep 12.
- Okuro RT, Morcillo AM, Ribeiro MÂ, Sakano E, Conti PB, Ribeiro JD. Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol. 2011 Jul-Aug;37(4):471-479. English, Portuguese. doi: 10.1590/s1806-37132011000400009.
- Perrotti G, Carrafiello A, Rossi O, Karanxha L, Baccaglione G, Del Fabbro M. Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients. Int J Environ Res Public Health. 2022 May 9;19(9):5751. doi: 10.3390/ijerph19095751. PMID: 35565146;
- Camacho M, Certal V, Abdullatif J, Zaghi S, Ruoff CM, Capasso R, Kushida CA. Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. 2015 May 1;38(5):669-675. doi: 10.5665/sleep.4652.
- Carrafiello A. Recovery of craniofacial proportions using the Nuvola Op System protocol. Journal of Oral Health and Craniofacial Science. December 2022;7(2):022–026. doi:10.29328/journal.johcs.1001041.
- Midori Albert A, Payne AL, Brady SM, Wright C. Craniofacial Changes in Children-Birth to Late Adolescence. ARC Journal of Forensic Science. 2019;4(1):1–19.
- Capote R, Preston K, Kapadia H. Craniofacial Growth and Development: A Primer for the Facial Trauma Surgeon. Oral Maxillofac Surg Clin North Am. 2023 Nov;35(4):501-513. doi: 10.1016/j.coms.2023.04.007.
- Bussu S. Nuvola aligners combined with a myofunctional device in paediatric treatment: A case report. 2023;2:38–44.
- Huang YS, Quo S, Berkowski JA, Guilleminault C. Short Lingual Frenulum and Obstructive Sleep Apnea in Pre-Pubertal Children. International Journal of Pediatric Research. 2015;1:003. doi: 10.23937/2469-5769/1510003.
- Align Technology. Align Technology Receives US FDA 510(k) Clearance for the Invisalign® Palatal Expander System to Address Skeletal and Dental Expansion in Growing Patients, Including Teenage Patients Which Represent the Majority of Orthodontic Case Starts Globally [Press Release]. Published: December 2023. https://investor.aligntech.com/news-releases/news-release-details/align-technology -receives-us-fda-510k-clearance-invisalignr.
- Yoon AJ, Zaghi S, Ha S, Law CS, Guilleminault C, Liu SY. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional – morphological study. Orthod Craniofac Res. 2017 Nov;20(4):237-244. doi: 10.1111/ocr.12206.
- Sadowsky C, Sakols EI. Long-term assessment of orthodontic relapse. Am J Orthod. 1982 Dec;82(6):456-463. doi: 10.1016/0002-9416(82)90312-8.
- Steinnes J, Johnsen G, Kerosuo H. Stability of orthodontic treatment outcome in relation to retention status: An 8-year follow-up. Am J Orthod Dentofacial Orthop. 2017 Jun;151(6):1027-1033. doi: 10.1016/j.ajodo.2016.10.032.
- Ojima K, Dan C, Schupp W, Kumagai Y. Invisalign Treatment Accelerated by Photobiomodulation. J Clin Orthod. 2016 May;50(5):309-317.
- Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012 Mar;141(3):289-297. doi: 10.1016/j.ajodo.2011.09.009.
- Guilleminault C, S Sullivan S. Towards Restoration of Continuous Nasal Breathing as the Ultimate Treatment Goal in Pediatric Obstructive Sleep Apnea. Enliven: Pediatrics and Neonatal Biology. 2014;1(1):01.
Besides craniofacial and respiratory issues, Dr. Olmos has also informed our readers about pediatric obstructive sleep apnea (POSA). Read more about the symptoms and possible therapies in our sister publication, Orthodontic Practice US, here: https://orthopracticeus.com/ce-articles/screening-and-treating-pediatric-osa/
